Tierra Walker had reached her limit. In the weeks since she’d learned she was pregnant, the 37-year-old dental assistant had been wracked by unexplained seizures and mostly confined to a hospital cot. With soaring blood pressure and diabetes, she knew she was at high risk of developing preeclampsia, a pregnancy complication that could end her life.
Her mind was made up on the morning of Oct. 14, 2024: For the sake of her 14-year-old son, JJ, she needed to ask her doctor for an abortion to protect her health.
“Wouldn’t you think it would be better for me to not have the baby?” she asked a physician at Methodist Hospital Northeast near San Antonio, according to her aunt. Just a few years earlier, Walker had developed a dangerous case of preeclampsia that had led to the stillbirth of her twins.
But the doctor, her family said, told her what many other medical providers would say in the weeks that followed: There was no emergency; nothing was wrong with her pregnancy, only her health.
Just after Christmas, on his birthday, JJ found his mom draped over her bed, lifeless. An autopsy would later confirm what she had feared: Preeclampsia killed her at 20 weeks pregnant.


Walker’s death is one of multiple cases ProPublica is investigating in which women with underlying health conditions died after they were unable to end their pregnancies.
Walker had known that abortion was illegal in Texas, but she had thought that hospitals could make an exception for patients like her, whose health was at risk.
The reality: In states that ban abortion, patients with chronic conditions and other high-risk pregnancies often have nowhere to turn.
They enter pregnancy sick and are expected to get sicker. Yet lawmakers who wrote the bans have refused to create exceptions for health risks. As a result, many hospitals and doctors, facing the threat of criminal charges, no longer offer these patients terminations, ProPublica found in interviews with more than 100 OB-GYNs across the country. Instead, these women are left to gamble with their lives.
As Walker’s blood pressure swung wildly and a blood clot threatened to kill her, she continued to press doctors at prenatal appointments and emergency room visits, asking if it was safe for her to continue the pregnancy. Although one doctor documented in her medical record that she was at “high risk of clinical deterioration and/or death,” she was told over and over again that she didn’t need to worry, her relatives say. More than 90 doctors were involved in Walker’s care, but not one offered her the option to end her pregnancy, according to medical records.
Walker’s case unfolded during the fall of 2024, when the dangers of abortion bans were a focus of protests, media coverage and electoral campaigns across the country. ProPublica had revealed that five women — three in Texas alone — had died after they were unable to access standard reproductive care under the new bans.
ProPublica condensed more than 6,500 pages of Walker’s medical records into a summary of her care with the guidance of two high-risk pregnancy specialists. More than a dozen OB-GYNs reviewed the case for ProPublica and said that since Walker had persistently high blood pressure, it would have been standard medical practice to advise her of the serious risks of her pregnancy early on, to revisit the conversation as new complications emerged and to offer termination at any point if she wanted it. Some described her condition as a “ticking time bomb.” Had Walker ended her pregnancy, every expert believed, she would not have died.
Many said that her case illustrated why they think all patients need the freedom to choose how much risk they are willing to take during pregnancy. Walker expressed that she didn’t want to take that risk, her family says. She had a vibrant life, a husband and son whom she loved.
Under Texas’ abortion law, though, that didn’t matter.

“I Don’t Know How Much More I Can Take”
On a hot September day, Walker was lying down with JJ after a walk with their two small dogs, Milo and Twinkie, when she started shaking uncontrollably.
Terrified, JJ called 911, asking for an ambulance.
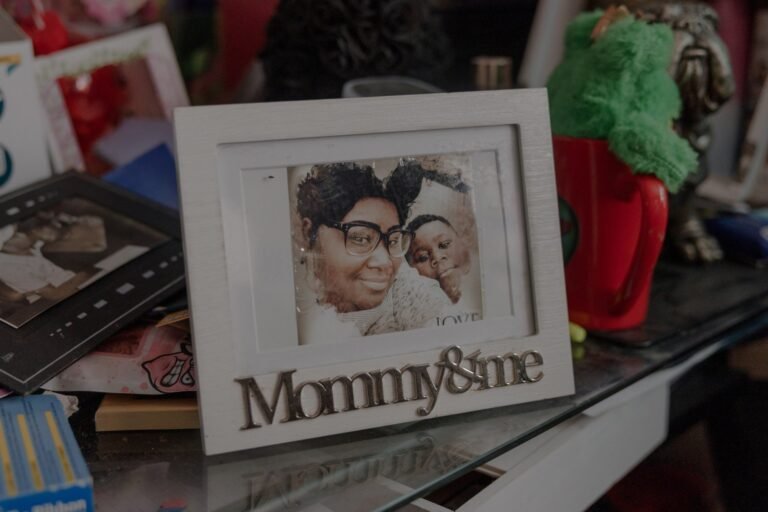
As the only child of a single mom, JJ had always considered Walker his closest friend, coach and protector wrapped in one. In their mobile home, JJ was greeted each morning by his mom’s wide smile and upturned eyes, as she shot off vocabulary quizzes or grilled him on state capitals. He loved how fearlessly she went after what she wanted; in 2021, she had proposed to her boyfriend, Eric Carson, and the two eloped. She’d just been talking about moving the family to Austin for a promotion she was offered at a dental clinic.


At the hospital, JJ was shocked to see her so pale and helpless, with wires snaking from her head and arms.
To Walker’s surprise, doctors quickly discovered that she was five weeks pregnant. They also noted hypertension at levels so high that it reduces circulation to major organs and can cause a heart attack or stroke. That, and her weight, age and medical history, put Walker at an increased risk of developing preeclampsia, a pregnancy-related blood pressure disorder, said Dr. Jennifer Lewey, director of the Penn Women’s Cardiovascular Health Program and expert in hypertension.
“If I’m seeing a patient in her first trimester and her blood pressure is this uncontrolled — never mind anything else — what I’m talking about is: Your pregnancy will be so high risk, do we need to think about terminating the pregnancy and getting your health under control?”
As Walker’s first trimester continued, she kept seizing. Her body convulsed, her eyes rolled back and she was often unable to speak for up to 30 minutes at a time. Some days, the episodes came in rapid waves, with little relief.
For three weeks, she stayed at Methodist hospitals; doctors were not able to determine what was causing the spasms. Walker couldn’t get out of bed, in case a seizure made her fall, and this left her vulnerable to blood clots. She soon developed one in her leg that posed a new lethal threat: It could travel to her lungs and kill her instantly.
Carson watched over her during the day and her aunt Latanya Walker took the night shift. She was panicked that her tough niece, whose constant mantra was “quit your crying,” now seemed defeated. One evening, during Walker’s third hospitalization, when she was about 9 weeks pregnant, she told Latanya she’d had a vision during a seizure: Her grandmother and aunt, who had died years earlier, were preparing a place for her on the other side.
“You better tell them you’re not ready to go,” Latanya said.
“I don’t know how much more I can take of this,” Walker whispered.

The next morning, Walker called for a doctor and asked about ending her pregnancy for the sake of her health. “When we get you under control, then everything will go smoothly,” the doctor replied, Latanya recalled. The physician on the floor was not an OB-GYN with the expertise to give a high-risk consultation, but the Walkers didn’t realize that this mattered. By the time the doctor left the room, her aunt said, tears streamed down Walker’s cheeks.
Dr. Elizabeth Langen, a maternal-fetal medicine specialist in Michigan who reviewed Walker’s case, said a physician comfortable with high-risk pregnancies should have counseled her on the dangers of continuing and offered her an abortion. “The safest thing for her was to terminate this pregnancy, that’s for sure.”
During Walker’s many hospital and prenatal visits, 21 OB-GYNs were among the more than 90 physicians involved in her care. None of them counseled her on the option — or the health benefits — of a termination, according to medical records.
In Texas, the law bars “aiding and abetting” an illegal abortion. As a result, many physicians have avoided even mentioning it, according to interviews with dozens of doctors.
In her condition, Walker couldn’t fathom leaving the state. When her aunt suggested ordering abortion medication online, Walker was worried she could go to jail. She was spending so much time in the hospital; what if she got caught taking the pills?
At 12 weeks pregnant, she was admitted to University Hospital. Doctors there noted that even on anticoagulation medication, the clotting in Walker’s leg was so profound that she needed a thrombectomy to remove it.
“At this point, we’ve gone from ‘complicated, but within the realm of normal’ to ‘we’ve got someone with a major procedure in pregnancy that tells us something isn’t going well,’” said Dr. Will Williams, a maternal-fetal medicine specialist in New Orleans, where an abortion ban is also in place. “In my practice, we’d have a frank discussion about whether this is a person we’d offer a termination to at the point of thrombectomy.”
ProPublica reached out to five physicians who were involved in key moments of Walker’s care: the hospitalist on duty on Oct. 14, 2024, when she asked about ending her pregnancy; three OB-GYNs; and a hospitalist on duty at the time of her thrombectomy. They did not respond. The hospitals Walker visited, including those run by University Health System and Methodist Healthcare, which is co-owned by HCA, did not comment on Walker’s care, despite permission from her family. Although the Walkers have not pursued legal action, they have engaged a lawyer. A University Health System spokesperson said that it is the company’s policy not to comment on potential litigation.
In her second trimester, Walker’s seizures continued and her hypertension remained out of control. At an appointment on Dec. 27, at around 20 weeks, a doctor noted spiking blood pressure and sent her to University Hospital’s ER. There, doctors recorded a diagnosis of preeclampsia.
The experts who reviewed Walker’s vital signs for ProPublica said her blood pressure of 174 over 115 was so concerning at that point, she needed to be admitted and monitored. Most questioned her doctor’s choice not to label her condition as severe. The treatment for severe preeclampsia, which points to a problem with the placenta, is delivery — or, at 20 weeks, an abortion.
Instead, doctors lowered her blood pressure with medication and sent her home.

Three days later, JJ crawled into bed with his mom and fed her soup. “I’m so sorry,” Walker croaked. “It’s your birthday and it shouldn’t be like this.”
He told his mom it was okay. He hadn’t expected laser tag or a trip to Dave & Buster’s this year. Over the past few months, when his mom was home, he had tried his best to make things easier on her, walking the dogs when she was out of breath, checking in every hour or so with a hug. JJ knew that after missing so many days of work, she had lost her job. She was stressed about getting enough food for the house. He was relieved when he heard her snoring — at least she was resting.
That afternoon, when his stepdad was out grocery shopping and his grandmother was just getting back from dialysis, he cracked open the door to Walker’s room.
His mom was lying face-down in bed, as if she had fallen over while getting up. JJ ran over and tried to find any sign she was breathing. When he called 911, a dispatcher coached him to slide her to the rug and start CPR.
“I need you,” he shouted as he leaned over his mom, pressing down on her chest. “I need you!”

“We Have to Allow for More Exceptions”
The anti-abortion activists who helped shape America’s latest wave of abortion bans have long seen health exemptions as a loophole that would get in the way of their goals. They fear such exceptions, if included in the laws, would allow virtually anyone to terminate a pregnancy.
In Idaho, an anti-abortion leader testifying at a state Senate hearing suggested doctors would use health exceptions to give abortions to patients with headaches.
In South Dakota, a pregnant Republican lawmaker with a high risk of blood clots begged her colleagues to consider creating a health exception that would protect her; her bill never made it to a hearing.
In Tennessee, an anti-abortion lobbyist with no medical training fought and defeated an amendment to the state law that would allow a health exception to “prevent” an emergency. He testified in the state Capitol that the carve-out was too broad since some pregnancy complications “work themselves out.”
The refusal to entertain these broader exceptions is particularly consequential given the state of women’s health. Women are entering pregnancy older and sicker than they have in decades. The rate of blood pressure disorders in pregnancy has more than doubled since 1993; they now affect up to 15% of U.S. pregnancies. And they’re most prevalent in states with restrictive abortion policies, according to a 2023 study in the Journal of the American College of Cardiology. The burden of disease falls heaviest on Black women, like Walker, for an array of reasons: neighborhood disinvestment, poor access to health care and discrimination in the medical system. Cuts to Medicaid funding and changes to the Affordable Care Act are likely to exacerbate these problems, according to experts.
Other countries give pregnant women and their doctors far more control over the medical decision to terminate. Across Europe, for example, most laws permit abortion for any reason through the first trimester, when more than 90% of abortions occur. After that gestational limit, their statutes also tend to include broad health exceptions that can be used for chronic conditions, illnesses that develop in pregnancy, fetal anomalies and, in some countries, mental health.
U.S. abortion bans generally restrict interventions to a far more limited set of health risks, like a “life-threatening medical emergency” or “substantial and irreversible” harm to major organs. A small subset of lawyers and doctors argue that the law can and should be interpreted to cover patients with chronic conditions that are worsening in pregnancy. But the vaguely written bans threaten criminal penalties for performing an illegal abortion — in Texas, up to 99 years behind bars. In practice, few hospitals grant health exceptions, ProPublica’s reporting has found.
Dr. Jessica Tarleton, an OB-GYN who provides abortions in South Carolina, recalled how much changed at her hospital when the state’s ban was put in place: OB-GYNs who want to provide an abortion to a patient with a health risk now need to get a maternal-fetal medicine specialist to explicitly write in the chart that it is necessary, in compliance with the law. Not many doctors are willing to do so.
“Some people were not because of their personal beliefs, and some because they didn’t want to be involved in any kind of potential legal actions,” Tarleton said. “They didn’t want their opinion to have anything to do with a patient getting an abortion or not.”
Recently, for example, Cristina Nuñez sued two hospitals in El Paso for their inaction in her care in 2023. She had diabetes, uncontrolled blood pressure and end-stage kidney disease when she learned she was unexpectedly pregnant at 36. Doctors wrote in her medical record that “she needs termination based on threat to maternal life or health,” but Nuñez alleged that one hospital failed to find an anesthesiologist willing to participate. She remained pregnant for weeks, even as blood clots turned her right arm black, until an advocacy organization threatened legal action and she was able to obtain an abortion. The lawsuit is ongoing.
This year, Texas Republicans passed legislation with minor amendments to their ban after ProPublica reported the deaths of three miscarrying women who did not receive critical abortion care during emergencies. In the updated law, an emergency still needs to be “life-threatening” to qualify for an abortion, but it no longer needs to be “imminent.” Doctors expect that most hospitals still won’t provide abortions to women like Walker who have dangerous chronic conditions but no certain threat to their lives.
ProPublica asked Sen. Bryan Hughes, the author of Texas’ abortion ban, about how the specific complications Walker faced should be treated by doctors under the amended law. When her pregnancy began, would she be eligible for an abortion due to her health? Would she need to wait for a diagnosis of severe preeclampsia? Is there a reason the law doesn’t include an exception for health risks? ProPublica put the same questions to the 20 state senators who co-wrote the bipartisan amendment.
Only Sen. Carol Alvarado, a Democrat, responded. In her view, the amendment was far too narrow. But, she said, her Republican colleagues defer to the far right of their base and oppose broader exceptions.
“You can’t proclaim to be pro-life, but you’re passing laws that are endangering women and causing death,” she said. “We have to allow for more exceptions.”

“So You’d Rather Let Somebody Die?”
After Walker died, her family felt bewildered by her medical care. The doctors had assured them that her baby was healthy and she would be fine. The autopsy found that the fetus was indeed healthy, at just under a pound and measuring 9 inches long. But it showed that Walker had hypertensive cardiovascular disease with preeclampsia, along with an enlarged heart, dangerously full of fluid, and kidney damage — signs that her condition had declined even more than she knew.
In Carson’s mind, the many doctors they saw cast the risks as challenges that would be overcome if his wife followed directions. “She was doing what they told her to do,” he said. He couldn’t understand how no one suggested ending the pregnancy to keep Walker safe. “Nobody said nothing.”
Latanya worried the law played a role. “They didn’t want to offer to end the pregnancy, because the government or someone says you can’t? So you’d rather let somebody die?” she said. “Now we are the ones that have to suffer.”
JJ couldn’t bear to stay in the home where he had found his mom, so he moved in with Latanya. Each day, he scrolls through old videos on the computer so he can hear Walker’s voice.
Latanya does everything she can to support him, but she knows she can’t erase his pain.
She recalls watching JJ steady himself at Walker’s funeral, to see her one last time. Until that point, he hadn’t cried.
When he finally faced the open casket where his mom lay holding her fetus, JJ sank to his knees, overcome. His aunt, uncles, cousins and grandmother gathered around him and rocked him in their arms.