South Africa has come a long way in the fight against HIV, boasting the world’s largest antiretroviral therapy (ART) programme. While the proportion of people living with HIV experiencing discrimination has decreased, stigma remains a major challenge for people living with HIV.
Findings from the 2024 HIV Stigma Index 2.0 report show that “more than half (54.6%) of those living with the virus have experienced the feeling of shame or guilt about their HIV positive status at some point in their lives”, says Duncan Moeketsi from the National Association of People Living with HIV and AIDS (NAPWA) and co-principal investigator during the launch of the study this week.
Subscribe to our newsletter
The report surveyed more than 5000 people over the age of 15 living with HIV in 18 health districts around the country. It showed a lack of trust in the healthcare system among key populations – people at an increased risk of HIV infection – including sex workers, men who have sex with men (MSM), and people who inject drugs. Twelve percent of people in this population say that they have, at some point, avoided health services.
On a positive note, 73,2% of the participants said they felt comfortable disclosing their status to family, which suggests that participants felt they would receive support and courage. More than 50% said they felt comfortable disclosing their status to friends and partners.
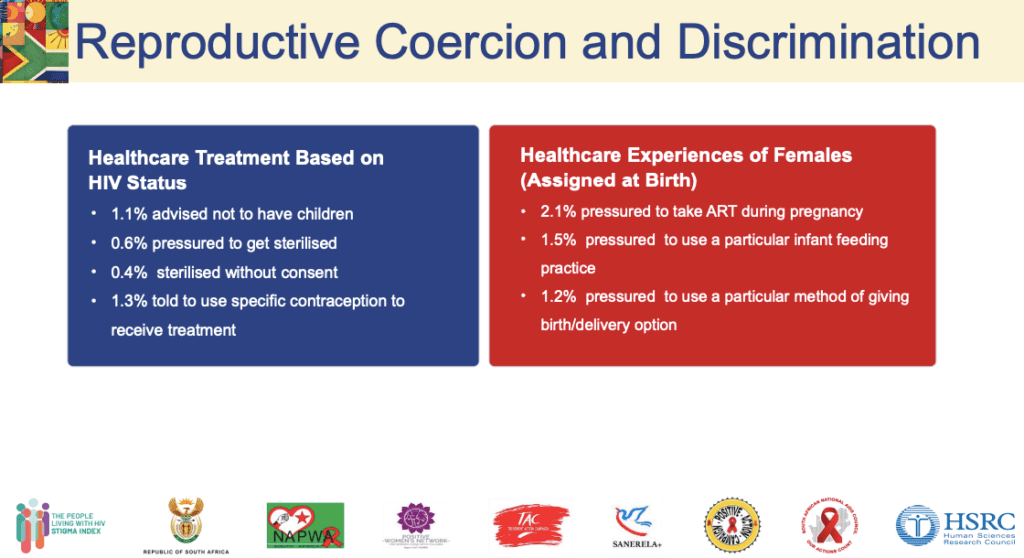
The researchers highlight areas of concern where participants reported cases of abuse and discrimination in public health facilities. Another major cause for alarm is reports by participants of being coerced into taking contraceptives or getting sterilised.
A closer look at the findings
Internalised stigma can lead to feelings of shame, fear of disclosure, isolation, and despair. These feelings were highest amongst men at 57.3% and 53% for women. Among young people aged 18-24, these feelings were 68.6%.
Overall, internalised stigma was higher amongst key populations: 65% of people who were using drugs experienced feeling shame or guilt about their status, followed by 60.3% of transgender people, 57.7% among MSM, and lastly 56.3% among sex workers.
People making up key populations were more likely to report discrimination or external stigma.
“Key populations have also reported physical harassment or being hurt based on either their sexual or gender identity. 12,9% of people who are using drugs said they experienced physical harassment or being hurt, making them the largest group among key populations experiencing this,” says Moeketsi.
Nearly a quarter (23%) of key populations said their family has either made discriminatory remarks or gossiped about them because of their HIV status. Around 1 in 5 (19%) felt excluded from family activities because of their HIV status, and 12.8% said they have been verbally harassed.
Even in healthcare settings, these groups don’t feel safe: 12% avoided healthcare services, and 8.7% say they’ve been concerned about their privacy or their confidentiality not being respected.
Concerning cases
Stigma in the healthcare setting continues to be an issue, with 3.2% of participants saying that they’ve been advised not to have sex because of their HIV status; 3.1% reported being talked badly about or being gossiped about. And 2% reported verbal abuse, including name-calling, yelling, and scolding.
“Even though the numbers are relatively small, with South Africa having made so much progress in terms of our [HIV] response, we should not be having these kinds of cases, ” says Moeketsi.
Alarmingly, women were the most affected by stigma and discrimination from healthcare workers, with 3 194 (8.3%) reporting experiencing stigma in health facilities. Of particular concern is that 1.1% of participants said they were told not to have children, and 2.1% reported being pressured to take ART during pregnancy.
Moeketsi says that ART is a cornerstone of HIV management, but it should come with information, and no one should be forced to take treatment if they are not ready.
“These are concerning cases. 0.6% of participants report being pressured to be sterilised. 0.4% have been sterilised without consent, while 1.3% told to use a specific contraception to receive treatment. It might look like a small number, but it’s very concerning and something that we need to pay attention to,” says Moeketsi.
Recommendations
Mluleki Zazini, National Chairperson of PLHIV, says people living with HIV, especially women-led organisations, must be at the forefront of designing and implementing all initiatives. He also shared that cultural sensitivity training is key.
“We need to deliver community-informed training modules for healthcare workers at healthcare facilities to provide stigma-free care, prioritising women, adolescent girls, sex workers, people who use drugs, and LGBTQ+,” he says.
In addition, the Department of Health, SANAC, along with networks of people living with HIV, need to design national awareness campaigns addressing psychological distress, low self-esteem, and reluctance to seek care.
“The Department of Social Development must provide resources for counselling and support groups, and the Department of Women, Youth and Persons with Disabilities must ensure gender-sensitive approaches to disclosure,” says Zazini. – Health-e News

